An interesting and provocative study, published last month in the journal Social Science and Medicine, suggests that the benefits of breastfeeding are overstated. In a clever experimental design, the authors analyzed data from a national database managed by the United States Department of labor’s Bureau of Labor Statistics. They queried from this database whether breastfeeding impacts any of the following outcomes in families with young siblings: body mass index, obesity, asthma, hyperactivity, parental attachment, behavioral compliance, reading comprehension, vocabulary recognition, math ability, memory based intelligence, and scholastic competence. They firstly looked at all families with siblings and noted that siblings who were breast fed fared better than their non-breastfed counterparts on all of the outcome variables measured except one; asthma rates were surprisingly higher among the breastfed siblings compared to the formula-fed siblings. When the authors looked specifically at families in which one sibling was breastfed but the other sibling was formula fed (this sub-analysis helps control for environmental variables other than breastfeeding that may explain the differences) they found that there were no differences between siblings in any of the outcomes measured. The authors conclude, therefore, that the benefits of breastfeeding are overstated.
The media and blogosphere followed suit with sensationalized headlines:
‘Breast milk no better than bottled,’ study claims
Are breastfeeding benefits overstated, overrated, or the healthiest way to go?
Hold the guilt! New study finds benefits of breastfeeding dramatically overstated.
Did this paper really demonstrate that breastfeeding isn’t as beneficial as we once thought? Well, I have a few comments to make in that regard:
Firstly, the ‘surprising’ asthma outcome is not really suprising. In recent decades, there has been a belief that breastfeeding is protective from asthma. Since asthma runs strongly in families, it is very possible that mothers who have strong histories or family histories of asthma are compelled to do whatever they can to prevent asthma in their children. Since it has been widely thought that breastfeeding is protective against asthma, it is plausible that mothers in this study with asthma and/or family histories of asthma were more likely to choose breastfeeding in an attempt prevent their children from developing asthma. Since these children were genetically more likely to develop asthma, many of them likely did develop asthma despite having been breastfeed. In this case, it was not the breastfeeding that increased the likelihood of developing asthma, it was the likelihood of developing asthma that increased the probability of the mother choosing to breastfeed her child. Though the analysis picked up on the connection, the design is only able to identify the correlation, not the direction of the cause nor if there is a causal relationship at all.
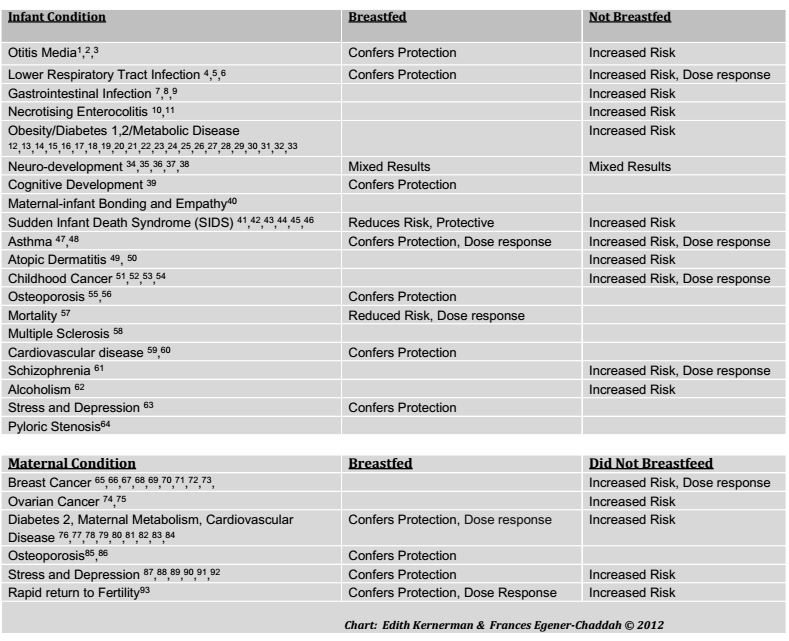
Secondly, the authors only looked at the impact of breastfeeding on the children; the maternal health benefits of breastfeeding such as protection from cancers, diabetes, cardiovascular disease, and mental health problems, were not considered at all.
Finally, I am suspicious of the outcome measures that were chosen by the authors. As one can see from the table below, there is no shortage of scientific literature demonstrating both the benefits of breastfeeding and the risks of formula feeding:
References are listed at the end of this post
If, from the list above, I selected the conditions for which there is the weakest connection between breastfeeding and protection from said conditions, I would choose asthma, obesity and neurocognitive development. In other words, current research has not been able to demonstrate very strongly that breastfeeding reduces the incidence of asthma, improves brain development, or protects from obesity. If those were the only reasons to promote breastfeeding, there wouldn’t be a very strong public health case to make for breastfeeding promotion. However, there are far more compelling reasons, as illustrated above, than those three outcome measures. Amazingly, the authors only chose those three specific outcomes (obesity, asthma, and a variety of neurocognitive outcomes) to measure in their study. It is almost as if the authors were rooting for a negative outcome at the onset of the study by picking outcome measures that were least likely to show any difference.
So, has this study demonstrated that formula feeding is the same as breastfeeding? I really don’t think so. And has this study demonstrated that the benefits of breastfeeding are overstated? For obesity, asthma, and cognitive outcomes: very possibly. But for the many other benefits that breastfeeding confers to both the child and the mother: not at all.
Chart references:
1. Duncan et al. Exclusive Breastfeeding for at least 4 Months Protects Against Otitis Media. Pediatrics, pp 867-872. Vol. 91, No. 5, May 1, 1993.
2. Ip S, Chung M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeed Med. 4(suppl):17–30, 2009.
3. Sheryl W. Abrahams and Miriam H. Labbok.Breastfeeding and Otitis Media: A Review of Recent Evidence Current Allergy and Asthma Reports, Volume 11, Number 6, Pages 508-512
4. Bachrach V, Schwarz E, Bachrach L. Breastfeeding and the Risk of Hospitalization for Respiratory Disease in Infancy: A Meta-analysis. Arch Pediatr Adolesc Med. 157(3):237-243. doi:10.1001/archpedi.157.3.237, 2003.
5. W. Oddy et al. Breastfeeding and Respiratory Morbidity in Infancy: A Birth Cohort Study. Arch Dis Child. 88 (3): 224-228, March, 2003.
6. Wilson et al. Relation of Infant Diet to Childhood Health: Seven Year Follow Up of Cohort of Children in Dundee Infant Feeding Study. British Medical Journal. Vol. 316, ISS: 7124. pp 21-25, 1998.
7. Chien PF, Howie. Breastfeeding and the risk of opportunistic infection in infancy in industrialized and non-industrialized settings. Adv Nutr Res. 10:69-104, 2001.
8. Kramer MS, Chalmers B Hodnett Ed, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): A randomized trial in the Republic of Belarus. JAMA. 285:413-420, 2001.
9. Quigley MA, Cumberland P, et al. How Protective is breast-feeding against diarrhoel diseases in infants in 1990s England? A Case-Control Study. Arch dis child. 91(3): 245-50, march, 2006. Epub 2005.
10. Ip S, et al 2009.
11. Holman RC, Stoll BJ, Curns AT et al. Necrotising enterocolitis hospitalizations among neonates in the United States. Paediatr Perinat Epidemiol. 20:498-506, 2006.
12. Arenz S, Rukerl R, Koletzko B, et al. Breastfeeding and childhood obesity- a systematic review. Int J Obes Relat Metab Disrd. 28:1247-1256, 2004.
13. Harder T, Bergmann R, Kallischnigg et al. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 165: 397-403, 2003.
14. Horta BL, Bahl R, Martines JC, et al. Evidence on long-term effect of breastfeeding: systematic review and meta-analyses. Geneva: World Health Organization: 1-57, 2007.
15. Taveras EM, Rifas-Shiman SL, Scanlon KS, Grummer-Strawn LM, Sherry B, Gillman MW. To what extent is the protective effect of breastfeeding on future overweight explained by decreased maternal feeding restriction?
Pediatrics. 2006 Dec;118(6):2341-8.
16. Olga Miralles, Juana Sánchez, Andreu Palou, Catalina Picó. A Physiological Role of Breast Milk Leptin in Body Weight Control in Developing Infants *Obesity (2006) 14, 1371–1377; doi: 10.1038/oby.2006.155
17. Owen CG, Whincup PH, Gilg JA et al. Effects of breastfeeding in infancy on blood pressure in later life: a systematic review and meta-analysis. BMJ. 327: 1189-1195, 2003.
18. Martin RM, Gunnell D, Smith GD, et al. Breastfeeding in infancy and blood pressure in later life: systematic review and meta-analysis. Am J Epidemiol. 161:15-26, 2005.
19. Owen CG, Martin RM, Whincup PH, et al. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 115:1367-1377, 2005.
20. Owen CG, Martin RM, Whincup PH, et al. Does breastfeeding influence risk of type 2 diabetes in later life? A quantitative review of published evidence. Am J Clin Nutr. 84:1043-1054, 2006.
21. Twells L, Newhook LA. Can exclusive breastfeeding reduce the likelihood of childhood obesity in some regions of Canada? Can J Public Health 2010;101(1):36-39
22. Stettler N, Stallings VA, Troxel AB, et al. Weight gain in the first week of life and overweight in adulthood: a cohort study of European American subjects fed infant formula. Circulation 2005;111:1897-1903.
23. Shim JE, Kim J, Mathai RA; STRONG Kids Research Team. Associations of infant feeding practices and picky eating behaviors of preschool children. J Am Diet Assoc. 2011 Sep;111(9):1363-8.
24. Shields L, Mamun AA, O’Callaghan M, Williams GM, Najman JM. Breastfeeding and obesity at 21 years: a cohort study. J Clin Nurs. 2010 Jun;19(11-12):1612-7.
25. Seach KA, Dharmage SC, Lowe AJ, Dixon JB. Delayed introduction of solid feeding reduces child overweight and obesity at 10 years. International Journal of Obesity 2010 Oct;34(10):1475-9
26. Musso G, Gambino R, Cassader M.Obesity, diabetes, and gut microbiota: the hygiene hypothesis expanded? Diabetes Care. 2010 Oct;33(10):2277-84.
27. Metzger MW, McDade TW. Breastfeeding as obesity prevention in the United States: A sibling difference model. Am J Human Biology 2010;22:291-296.
28. Martens PJ. What do Kramer’s Baby Friendly Hospital Initiative PROBIT studies tell us? A review of a decade of research. Journal of Human Lactation 2012 Aug;28(3):335-42.
29. Mangrio E, Lindström M, Rosvall M. Early life factors and being overweight at 4 years of age among children in Malmö, Sweden. BMC Public Health. 2010 Dec 15;10:764.
30.L i R, Magadia J, Fein SB, Grummer-Strawn LM. Risk of Bottle-feeding for Rapid Weight Gain During the First Year of Life. Arch Pediatr Adolesc Med. 2012 May;166(5):431-6.
31. Karanja N, Lutz T, Ritenbaugh C, Maupome G, Jones J, Becker T, Aickin M. The TOTS community intervention to prevent overweight in American Indian toddlers beginning at birth: A feasibility and efficacy study. J Community Health. 2010 Dec;35(6):667-75.
32. Shim JE, et al 2011
33. Scott JA, Ng SY, Cobiac L. The relationship between breastfeeding and weight status in a national sample of Australian children and adolescents. BMC Public Health. 2012 Feb 7;12:107.
34. Anderson JW, Johnstone BM, Remley DT. Breastfeeding and cognitive development: a meta-analysis. Am J Clin Nutr. 70: 525-535, 1999.
35. Stuebe, Alison. The Risks of Not Breastfeeding for Mothers and Infants. Reviews in Obstetrics and Gynecology. Vol.2 No. 4, 2009.
36. Jain A, Concato J, Leventhal JM. How good is the evidence linking breastfeeding and intelligence? Pediatrics. 109:1044-1053, 2002.
37. Drane DL, Logemann JA. A critical evaluation of the evidence on the association between type of infant feeding and cognitive development. Paediatr Perinat Epidemiol. 14:349-356, 2000.
38. Dewey KG, Cohen RJ, Brown KH, et al. Effects of exclusive breastfeeding for four versus six months on maternal nutritional status and infant motor development: results of two randomized trials in Honduras. J Nutr. 131: 262-267, 2001.
39. Kramer MS, et al 2001.
40. Kim P et al. J Child Psych Psychiatry, 2011
41. M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeed Med. 4(suppl):17–30, 2009.
Breastfeeding and the Risk of Postneonatal Death in the United States
42. Aimin Chen and Walter J. Rogan Pediatrics 2004;113;e435.
43. McVea KL, Turner PD, Peppler DK. The role of breastfeeding in sudden infant death syndrome. J Hum Lact. 16:13-20, 2000
44. American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome. The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 116: 1245-1255, 2005
45. McKenna, J. J., Ball, H. L. and Gettler, L. T. (2007), Mother–infant cosleeping, breastfeeding and sudden infant death syndrome: What biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am. J. Phys. Anthropol., 134: 133–161. doi: 10.1002/ajpa.20736
46. Vennemann MM, Bajanowski T, Jorch G, Mitchell EA. Does Breastfeeding reduce the Risk of Sudden Infant Death Syndrome?” Pediatrics Vol.123, March 2009, pp e406-410
47. Ip S, et al, 2009.
48. Ip S. et al. Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. US AHRQ. 2007
49. Gdalevich M, Mimouni D, David M, et al. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol. 45: 520-527, 2001.
50. Kramer MS, et al, 2001.
51. C Svanborg, A Aits, P Brest et al. HAMLET, a tumoricidal molecular complex form human milk. BioMed Central. 3 (suppl 5): S11, 2009.
52. Greaves MF. Speculation on the cause of childhood lymphoblastic leukemia: a meta-analysis. Leukemia. 2: 120-125, 1988.
53. Ip S, Chung M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality’s evidence report on
54. Schraw J, et al “Longer formula feeding and later age at introduction of solids increase the odds ratio of pediatric acute lymphoblastic leukemia” AACR-FCPR 2012; Abstract A102.
55. Bishop NJ, Dahlenburg SL, Fewtrell MS, et al. Early diet of preterm infants and bone mineralization at age five years. Acta Pædiatr 1996;85:230-6
56. Ryan S. Bone mineralization in Preterm Infants. Nutrition. 1998;14:745-747
57. Aimin Chen, MD, PhD, Walter J. Rogan, MD Breastfeeding and the Risk of Postneonatal Death in the United States PEDIATRICS Vol. 113 No. 5 May 1, 2004 Pp. E435 -e439
58. Conradi S, Malzahn U, Paul F, Quill S, Harms L, Then Bergh F, Ditzenbach A, Georgi T, Heuschmann P, Rosche B. Breastfeeding is associated with lower risk for multiple sclerosis. Mult Scler. 2012 Sep 4
59. Williams, M. J. A., Williams, S. M., & Poulton, R. (2006). Breast feeding is related to C-reactive protein concentration in adult women. Journal of Epidemiology and Community Health, 60, 146-148
60. Brion MJ, Lawlor DA, Matijasevich A, Horta B, Anselmi L, Araújo CL, Menezes AM, Victora CG, Davey Smith G What are the causal effects of breastfeeding on IQ, obesity and blood pressure? Evidence from comparing high-income with middle-income cohorts. Int J Epidemiol. 2011 Feb 24. [Epub ahead of print]
61. H. J. Sørensen, E. L. Mortensen, J. M. Reinisch, S. A. Mednick. Breastfeeding and risk of schizophrenia in the Copenhagen Perinatal Cohort.
62. Acta Psychiatr Scand. 2005 July; 112(1): 26–29. doi: 10.1111/j.1600-0447.2005.00548.x
63. Sørensen HJ, Mortensen EL, Reinisch JM, Mednick SA. Early weaning and hospitalization with alcohol-related diagnoses in adult life. Am J Psychiatry. 2006 Apr;163(4):704-9.
64. Montgomery, S. M., Ehlin, A., & Sacker, A. (2006). Breast feeding and resilience against psychosocial stress. Archives of Diseases of Childhood, 91, 990-994
65. Krogh, C et al. Bottle-feeding and the Risk of Pyloric Stenosis. Pediatrics, Sept 2012 online
66. Stuebe AM, Willet WC, Xue F, et al. Lactation and incidence of premenopausal breast cancer: a longitudinal study. Arch Intern Med. 169:1364-1371, 2009.
67. Tryggvadóttir L, Tulinius H, Eyfjord JE, et al. Breastfeeding and reduced risk of breast cancer in an Icelandic cohort study. Am J Epidemiol.154:37-42, 2001.
68. Michels KB, Willet WC, Rosner BA, et al. Prospective assessment of breastfeeding and breast cancer incidence among 89,887 women. Lancet. 347:431-436, 1996.
London SJ, Colditz GA, Stampfer MJ, et al. Lactation and risk of breast cancer in a cohort of US women. Am J Epidemiol.132:17-26.1990.
69. Stuebe, Alison et al Arch Intern Med 2009;
70. Lee SY, Kim MT, Kim SW, et al. Effect of lifetime lactation on breast cancer risk: a Korean women’s cohort study. Int J Cancer. 105: 390-393, 2003.
71. Kvale G, Heuch I. Lactation and cancer risk: is there a relation specific to breast cancer? J Epidemiol Community Health. 42:30-37,1988.
72. Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and women without the disease. Lancet. 360:187-195, 2002.
73. Bernier MO, Plu-Bureau G, Bossard N, et al. Breastfeeding and risk of breast cancer: a meta- analysis of published studies. Hum Reprod Up- date. 6:374-386, 2000.
74. Cramer DW, Titus-Ernstoff L, McKolanis JR, et al. Conditions associated with antibodies against the tumor-associated antigen MUC1 and their relationship to risk for ovarian cancer. Cancer Epidemiol Biomarkers Prev.14: 1125-1131,2005
75. Danforth KN, Tworoger SS, Hecht JL, et al. Breastfeeding and risk of ovarian cancer in two prospective cohorts. Cancer Causes Control.18:517-523, 2007
76. Kac G, Benício MHDA, Velásquez-Meléndez G, Joaquim et al. Breastfeeding and postpartum weight retention in a cohort of Brazilian women. Am J Clin Nutr, 2004; 79: 487 – 493
Olga Miralles, et al. 2006
77. Stuebe AM, Michels KB, Willett WC, et al. Duration of lactation and incidence of myocardial infarction in middle to late adulthood. Am J Obstet Gynecol. 200:138.e1-e8. 2009.
78. Stuebe AM, Rich-Edwards JW, Willett WC, et al. Duration of lactation and incidence of type 2 diabetes. JAMA. 294:2601-2610, 2005.
79. Dewey KG, Heinig MJ, Nommsen LA. Maternal weight-loss patterns during prolonged lactation. Am J Clin Nutr. 58:162-166, 1993.
80. Schwarz EB, Ray RM, Stuebe AM, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol. 113:974-982, 2009.
81. Stuebe AM, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 26:81-88, 2009.
82. Eleanor Bimla Schwarz, MD, MS, Roberta M. Ray, MS, Alison M. Stuebe, MD, MSc,
83. Matthew A. Allison, MD, MPH, Roberta B. Ness, MD, MPH, Matthew S. Freiberg, MD, MSc, and Jane A. Cauley, DrPH Duration of Lactation and Risk Factors forMaternal Cardiovascular Disease
84. Ram KT, Bobby P, Hailpern SM, et al. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife-SWAN, the study of women’s health across the nation. Am J Obstet Gynecol. 198:268.e1-e6, 2008.
85. Chantry CJ, Auinger P, Byrd RS. Lactation among adolescent mothers and subsequent bone mineral density. Arch Pediatr Adolesc Med 2004;158:650-6
86. Ward et al. Curr Opin Obstet Gynecol. 2005
87. Groer, M. W. (2005). Differences between exclusive breastfeeders, formula-feeders, and controls: A study of stress, mood, and endocrine variables. Biological Nursing Research, 7(2), 106-117
88. Groër, M. W., Davis, M.W., Smith, K., Casey, K., Kramer, V., & Bukovsky, E. (2005). Immunity, inflammation and infection in post-partum breast and formula feeders. American Journal of Reproductive Immunology, 54, 222-231
89. Groer, M. W., & Davis, M. W. (2006). Cytokines, infections, stress, and dysphoric moods in breastfeeders and formula feeders. Journal of Obstetric, Gynecologic and Neonatal Nursing, 35, 599-607
90. Heinrichs, M., Meinlschmidt, G., Neumann, I., Wagner, S., Kirschbaum, C., Ehlert, U., et al. (2001). Effects of suckling on hypothalamic-pituitary-adrenal axis responses to psychosocial stress in postpartum lactating women. Journal of Clinical Endocrinology & Metabolism, 86, 4798-4804
91. Kendall-Tackett, K. A new paradigm for depression in new mothers: The central role of inflammation and how breastfeeding and anti-inflammatory treatments protect maternal mental health. International Breastfeeding Journal, 2:6( http://www.internationalbreastfeedingjournal.com/content/2/1/6) .2007
92. Peus V, Redelin E, Scharnholz B, Paul T, Gass P, Deuschle P, Lederbogen F, Deuschle M: Breast-Feeding in Infancy and Major Depression in Adulthood: A Retrospective Analysis. Psychother Psychosom 2012;81:189-190
93. McNeilly A. Endocrinol Metab Clin North Am. 1993 Mar;22(1):59-73
